Polyvagal Theory: Advancing the Understanding of the Autonomic Nervous System in Medicine
Introduction
In the previous blog post, we touched upon the application of polyvagal theory in primary care medicine and how it provides a framework for understanding patients’ reactions that can influence their medical problems. Now, let’s delve deeper into the background of polyvagal theory and how it has advanced our understanding of the autonomic nervous system (ANS). This groundbreaking theory was developed by Dr. Stephen Porges, an influential figure in the field of neuroscience and psychophysiology.
Dr. Stephen Porges and the Polyvagal Theory
In traditional medical school teachings, the ANS is often presented as a simple dichotomy, consisting of the sympathetic and parasympathetic branches. The sympathetic branch is associated with the “fight-or-flight” response, while the parasympathetic branch is associated with “rest and digest” functions. While this teaching has provided a basic understanding of the ANS, Dr. Porges has provided another comprehensive explanation.
Dr. Stephen Porges, a renowned researcher and professor of psychiatry, has revolutionized our understanding of the ANS with his polyvagal theory. His work represents a significant shift in our comprehension of autonomic functioning and its implications for human behavior and health.
Background of Dr. Porges
copied from the website www.stephenporges.com
“Dr. Porges is a Distinguished University Scientist at Indiana University where he is the founding director of the Traumatic Stress Research Consortium. He is Professor of Psychiatry at the University of North Carolina, and Professor Emeritus at both the University of Illinois at Chicago and the University of Maryland.
He served as president of the Society for Psychophysiological Research and the Federation of Associations in Behavioral & Brain Sciences and is a former recipient of a National Institute of Mental Health Research Scientist Development Award. He has published more than 400 peer-reviewed papers across several disciplines including anesthesiology, biomedical engineering, critical care medicine, ergonomics, exercise physiology, gerontology, neurology, neuroscience, obstetrics, pediatrics, psychiatry, psychology, psychometrics, space medicine, and substance abuse. In 1994 he proposed the Polyvagal Theory, a theory that links the evolution of the mammalian autonomic nervous system to social behavior and emphasizes the importance of physiological state in the expression of behavioral problems and psychiatric disorders. The theory is leading to innovative treatments based on insights into the mechanisms mediating symptoms observed in several behavioral, psychiatric, and physical disorders.
He is the author of The Polyvagal Theory: Neurophysiological foundations of Emotions, Attachment, Communication, and Self-regulation (Norton, 2011), The Pocket Guide to the Polyvagal Theory: The Transformative Power of Feeling Safe, (Norton, 2017), co-editor of Clinical Applications of the Polyvagal Theory: The Emergence of Polyvagal-Informed Therapies (Norton, 2018) and author of Polyvagal Safety: Attachment, Communication, Self-Regulation (Norton 2021). Dr. Porges is the creator of a music-based intervention, the Safe and Sound Protocol ™ (SSP), which is used by therapists to improve social engagement, language processing, and state regulation, as well as to reduce hearing sensitivities.”
Polyvagal theory was developed by integrating research findings from various disciplines, including neuroscience, physiology, psychology and evolutionary biology
To understand how polyvagal theory can be used as a backdrop for looking at how its precepts can be used to understand how the autonomic nervous system plays a major role in the pathophysiology of many medical problems faced in primary care, we first need to discuss the evolution of polyvagal theory through Dr. Porges and his associates.
In 1992, Dr. Porges proposed that measuring respiratory sinus arrhythmia (RSA) could be used as an index of stress vulnerability in clinical medicine (1).
Unlike traditional measures of heart rate variability, the focus was on RSA, which represents the neural origin and functional output from the vagus nerve to the heart, known as cardiac vagal tone. It was suggested that RSA would provide a more sensitive indicator of health status compared to global measures of heart rate variability, which involve both neural and non-neural factors. The paper introduced a quantitative approach using time-series analysis to extract the amplitude of RSA as a more accurate measure of vagal activity. Data presented in the article demonstrated that healthy full-term infants had significantly greater RSA amplitude than preterm infants. While the idea of using heart rate patterns to assess vagal activity had been reported as early as 1910 (2).
The paper provided further evidence, and subsequent studies have consistently shown that blocking the vagus nerve with atropine decreases RSA in mammals (3,4).
After reading the mentioned article (4) a neonatologist sent Dr. Porges a letter expressing concern. He mentioned that during his medical studies, he learned that excessive vagal tone could be dangerous, specifically citing the risk of neurogenic bradycardia. This condition, characterized by a slow heart rate, can indicate fetal distress during delivery. The neonatologist also highlighted that bradycardia and apnea are significant indicators of risk for newborns. Thus, there seemed to be two important responses mediated by the vagus nerve.
To understand this puzzling finding, Dr, Porges and his colleagues conducted further research on human fetuses during delivery. They discovered that fetal bradycardia, a slow heart rate, only occurred when respiratory sinus arrhythmia was reduced. Interestingly, they observed that the fetal heart showed a respiratory rhythm even without the typical chest movements associated with breathing after birth (5).
This raised an important question: How could vagal mechanisms be responsible for both respiratory sinus arrhythmia, which is protective, and bradycardia, which can be dangerous? This inconsistency led to what they called the “vagal paradox” and became the driving force behind the development of polyvagal theory.
There is a clear contradiction between the data and the physiological assumptions regarding the mechanism that control bradycardia and heart rate variability. Physiological models assume that the vagus nerve regulates both the heart rate and amplitude of respiratory sinus arrythmia (6,7).
Studies have consistently shown that vagal fibers responsible for inhibiting the heart exhibit bradycardia and a respiratory rhythm when stimulated. However, there are instances where these measures do not align, indicating independent neural control sources. Examples include bradycardic episodes related to hypoxia, vasovagal syncope, and fetal distress. Despite these observable phenomena, some researchers argue for a correlation between these two parameters, assuming a single central vagal source. This inconsistency, which arises from this assumption, is what Dr. Porges refers to again as the vagal paradox.
The three phylogenetic stages outlined in polyvagal theory: the ventral vagal complex, sympathetic fight-or-flight response, and dorsal vagal complex
Dr. Porges has gone on to explain that understanding the evolutionary development of the autonomic nervous system in vertebrates helps unravel the vagal paradox. Through comparative studies of neuroanatomy and neurophysiology, two distinct branches of the vagus nerve have been identified, each serving distinct adaptive functions and behavioral strategies. One branch of the vagus nerve controls respiratory sinus arrhythmia, while the other branch is responsible for bradycardia and potentially slower rhythms in heart rate variability. Despite assumptions that these slower rhythms are influenced by the sympathetic nervous system, they are actually blocked by atropine (4). This knowledge sheds light on the different roles played by each branch of the vagus nerve in regulating heart function.
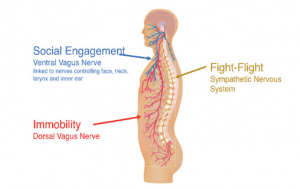
The polyvagal theory, (4,8, 9, 10, 11, 12) provides insights into the development of the autonomic nervous system in vertebrates, highlighting three stages that are associated with distinct autonomic subsystems found in mammals. These subsystems are organized in a phylogenetic order and are closely related to specific behaviors. The first subsystem (ventral vagal system) is linked to social communication, involving facial expression, vocalization, and listening. The second subsystem (sympathetic system) is associated with mobilization, which includes fight-or-flight responses. Lastly, the third subsystem (dorsal vagal system) is related to immobilization, which encompasses behaviors such as feigning death, vasovagal syncope, and behavioral shutdown (dissociation). This theory helps us understand how these autonomic subsystems evolved and their role in different behavioral contexts.
Adapted from “Perspective on Complex Trauma” The Journal of the Complex Trauma Institute.
The social communication system, also known as the social engagement system, involves the myelinated vagus (dorsal vagal). This system promotes calm behavioral states by inhibiting sympathetic influences on the heart and reducing activity in the hypothalamic-pituitary-adrenal (HPA) axis (13).
The mobilization system relies on the sympathetic nervous system for its functioning. The most primitive component, the immobilization system, relies on the unmyelinated vagus, which is shared among most vertebrates. As neural complexity increases through phylogenetic development, the organism’s behavioral and emotional capabilities become more diverse. These three systems work dynamically to provide adaptive responses to safe, dangerous, and life-threatening situations.
The myelinated vagus (ventral vagal) is unique to mammals and originates in the nucleus ambiguus, with preganglionic nicotinic receptors and postganglionic muscarinic receptors. In contrast, the unmyelinated vagus (dorsal vagal), present in reptiles, amphibians, teleosts, and elasmobranchs, originates in the dorsal motor nucleus of the vagus and has both pre- and postganglionic muscarinic receptors.
Dr. Porges and his colleagues in the past have been researching the possibility of using different features of the heart rate pattern to monitor the two vagal systems dynamically. Preliminary studies conducted in their laboratory, using prairie voles with high vagal tone, have shown promising results. By blocking nicotinic preganglionic receptors with hexamethonium and muscarinic receptors with atropine, they have observed that respiratory sinus arrhythmia was selectively removed without significantly affecting the lower frequencies in heart rate variability. In contrast, blocking muscarinic receptors with atropine eliminated both the low and respiratory frequencies (14). With these studies they have further delineated a separation of the two different vagal activities.
The Hierarchal Separation of These Three Distinct Circuits
The three circuits in the autonomic nervous system are organized in a hierarchy determined by evolution, following the principle of dissolution proposed by Jackson (15). According to Jackson’s principle, higher neural circuits inhibit lower neural circuits, and when the higher circuits are impaired, the lower circuits become more active. While Jackson applied this concept to explain brain function changes due to damage or illness, the polyvagal theory suggests a similar hierarchical model for autonomic responses to challenges.
In terms of function, when the environment is perceived as safe, two important features are observed. Firstly, the body’s state is regulated efficiently to promote growth and restoration, maintaining visceral homeostasis. This involves an increased influence of the mammalian myelinated vagal motor pathways (ventral vagal) on the heart’s pacemaker, resulting in a slower heart rate, inhibition of fight-or-flight responses from the sympathetic nervous system, suppression of the stress response system involving the hypothalamic-pituitary-adrenal (HPA) axis (including cortisol release), and modulation of immune reactions (such as cytokine levels) to reduce inflammation. Secondly, throughout evolution, the brainstem nuclei responsible for regulating the myelinated vagus became integrated with the nuclei controlling the muscles of the face and head. This connection led to a bidirectional relationship between spontaneous social engagement behaviors and bodily states. Specifically, in mammals, the integration of neural regulation of visceral states promoting growth and restoration (via the myelinated vagus) with the neural regulation of muscles controlling eye gaze, facial expressions, listening, and prosody resulted in the emergence of an integrated social engagement system.
This interconnected system allows for coordinated responses between physiological states and social behaviors, contributing to overall well-being in safe environments (4). The human nervous system, like that of other mammals, has evolved not only to function in safe environments but also to ensure survival in dangerous and life-threatening situations. To achieve this adaptability, the human nervous system has retained two more primitive neural circuits that regulate defensive strategies, including fight-or-flight responses and death-feigning behaviors. It’s important to note that these defensive behaviors are incompatible with social behavior, social communication, and maintaining internal bodily balance.
As a result, the human nervous system maintains three neural circuits organized in a phylogenetic hierarchy. In this hierarchy of adaptive responses, the newest circuit is activated first. If this circuit fails to provide safety, the older circuits are sequentially recruited to deal with the threat. This organization allows for flexible and effective responses to different challenges and ensures survival in various contexts.
Through the study of the evolution of heart regulation in vertebrates (8,9,16,17) four key principles have been identified that can be used to test hypotheses regarding specific neural mechanisms and their relation to social engagement, fight-or-flight responses, and death-feigning behaviors:
- Phylogenetic shift in heart regulation: The regulation of the heart has evolved from endocrine communication to unmyelinated nerves, and finally to myelinated nerves.
- Development of opposing neural mechanisms: There is a development of neural mechanisms that both excite and inhibit the heart, allowing for rapid and graded regulation of metabolic output.
- Face-heart connection: A connection between the face and heart has evolved, with the source nuclei of the vagal pathways shifting to the nucleus ambiguous. This anatomical and neurophysiological linkage between the neural regulation of the heart through the myelinated vagus and the pathways controlling the facial and head muscles has formed an integrated social engagement system.
- Increased cortical control: With increased cortical development, the cortex has greater control over the brainstem through direct (corticobulbar) and indirect (corticoreticular) neural pathways. These pathways originate in the motor cortex and terminate in the source nuclei of the myelinated motor nerves emerging from the brainstem. This control extends to visceromotor structures (such as the heart and bronchi) as well as somatomotor structures (muscles of the face and head).
These principles provide a foundation for understanding the neural mechanisms involved in different behaviors and allow for further investigation into the regulation of the heart in relation to social engagement, fight-or-flight responses, and death-feigning behaviors.
In order to transition from defensive behaviors to social engagement strategies, the mammalian nervous system must accomplish two essential tasks:
- assess the level of risk, and
- if the environment is perceived as safe, inhibit the more primitive limbic structures that control fight, flight, or freeze responses.
Any stimulus that signals safety has the potential to activate the evolutionarily advanced neural circuits responsible for promoting prosocial behaviors within the social engagement system.
Neuroception our Powerful Subconscious Mind
The nervous system continually evaluates risk by processing sensory information from the environment and internal organs. This evaluation does not require conscious awareness and involves subcortical limbic structures (18).
To highlight this distinct neural process, the term “neuroception” was introduced by Dr. Porges (19).
Neuroception allows the nervous system to distinguish between features in the environment (and within the body) that are safe, dangerous, or life-threatening. In safe environments, the autonomic state is regulated to reduce sympathetic activation and protect the oxygen-dependent central nervous system, particularly the cortex, from the more conservatively reactive responses of the dorsal vagal complex.
However, how does the nervous system determine when the environment is safe, dangerous, or life-threatening, and which neural mechanisms are involved in this risk assessment?
Neuroception is a neural process that allows humans and other mammals to engage in social behaviors by distinguishing between safe and dangerous situations. It is considered a mechanism that influences positive social behavior, emotional regulation, and maintaining bodily balance (4, 19).
Neuroception is believed to be triggered by feature detectors in the temporal cortex, which communicate with the central nucleus of the amygdala and the periaqueductal gray. This communication helps modulate limbic reactivity based on responses to voices, faces, and hand movements. The neuroception of familiar individuals and those with warm, expressive faces and appropriate vocal tone promotes a sense of safety, facilitating social interactions.
In most individuals, the nervous system effectively evaluates risk and adjusts the physiological state accordingly to match the actual risk in the environment. When the environment is perceived as safe, the defensive limbic structures are inhibited, allowing for social engagement and a state of calmness. However, some individuals experience a mismatch where the nervous system appraises the environment as dangerous even when it is safe. This mismatch leads to physiological states that support fight, flight, or freeze responses, but hinder social engagement behaviors. According to the theory, effective social communication can occur through the social engagement system only when these defensive circuits are inhibited. In this world of multiple stressors, it’s no wonder the traditions brought about by social communication have deteriorated.
The perception of risk in the environment is not solely driven by external factors. Feedback from the internal organs, known as afferent feedback from the viscera, plays a significant role in influencing the accessibility of prosocial circuits associated with social engagement behaviors. According to the polyvagal theory, states of mobilization, such as when the body is in a heightened state of readiness, can hinder our ability to detect positive social cues. Visceral states also influence our perception of objects and other individuals. As a result, the same social interactions can lead to different outcomes depending on the physiological state of the person involved. If the individual is in a state where the social engagement system is easily accessible, positive reciprocal interactions are more likely to occur. However, if the person is in a state of mobilization, the response may be withdrawal or aggression instead of engaging socially. In this state, it can be challenging to dampen the mobilization circuit and re-engage the social engagement system.
The insula, a brain structure, may play a role in mediating neuroception. It has been suggested that the insula is involved in processing the diffuse feedback from the viscera and bringing it into cognitive awareness. Functional imaging studies have demonstrated the insula’s involvement in various experiences, including pain and emotions such as anger, fear, disgust, happiness, and sadness. Researcher Critchley proposes that the insula represents internal body states and contributes to subjective feelings. Additionally, studies have shown a correlation between insula activity and interoceptive accuracy, which refers to the ability to accurately perceive and interpret bodily sensations (21).
The Ventral Vagus System as the Social Engagement System
Understanding the three phylogenetic stages outlined in the polyvagal theory – the ventral vagal complex, sympathetic fight-or-flight response, and dorsal vagal complex – provides crucial insights into the evolution and functioning of the autonomic nervous system. While each stage has its own adaptive significance, it is the ventral vagal complex that holds practical relevance in maintaining the homeostasis of the human species. This stage is associated with the social engagement system, which encompasses a range of behaviors and physiological processes related to social interaction, emotional regulation, and visceral homeostasis. Exploring the practical applications of the ventral vagal complex, the social engagement system holds promise for understanding and enhancing human well-being in various contexts, including relationships, communication, and overall physical and emotional health.
The social engagement system is a crucial component of the autonomic nervous system and is responsible for feelings of safety and connection. According to the polyvagal theory, the social engagement system is a distinct branch of the autonomic nervous system that works in conjunction with the sympathetic and parasympathetic systems to regulate various physiological functions in the body (21). The social engagement system is primarily mediated by the vagus nerve, which is a cranial nerve that connects the brainstem to the heart, lungs, and digestive system (21).
The ventral vagal complex, a group of structures in the brainstem that regulates social behavior, is responsible for activating the social engagement system. When the social engagement system is activated, the body enters a state of calmness and relaxation that promotes social interaction and co-regulation (4).
The social engagement system plays a critical role in promoting physical and emotional health. By activating the social engagement system, individuals can experience feelings of safety, trust, and connectedness, which are essential for building and maintaining social relationships. Social support has been linked to improved immune function, reduced stress levels, and increased longevity (22).
In contrast, the absence of social support can lead to social isolation, which has been linked to numerous health problems, including depression, anxiety, cardiovascular disease, and immune dysfunction (23).
Moreover, chronic stress and trauma can dysregulate the social engagement system, leading to a chronic state of hypervigilance that impairs social functioning and exacerbates stress-related disorders (21). It is this chronic state of hypervigilance that puts people in a state of threat awareness that can worsen pathology.
Co-regulation as a Crucial Component of the Social Engagement System
Co-regulation is a crucial component of the social engagement system, which is part of the ventral vagal complex in the polyvagal theory. It refers to the reciprocal and synchronized regulation of physiological and emotional states between individuals during social interactions. In co-regulation, the nervous systems of two or more individuals interact in a way that supports mutual well-being and emotional connection. The concept of co-regulation gained recognition as we started to comprehend the mutual influence between a developing baby and its mother. Even before birth, the baby begins to hear and recognize its mother’s voice, which becomes a comforting sound. As an infant, the baby associates the voice with a parent’s smiling face, and as a toddler, they learn to seek regulation from their parents in various situations, such as after a fall or when feeling distressed. This process demonstrates the early stages of co-regulation, where the baby relies on the presence and cues from their caregiver to find comfort and regulation in their emotional and physiological states.
Within the social engagement system, co-regulation plays a vital role in fostering positive social interactions and promoting a sense of safety, trust, and emotional resilience. When individuals engage in co-regulation, their physiological states, including heart rate, respiration, and emotional arousal, can become synchronized. This synchronization often occurs through nonverbal cues, such as facial expressions, tone of voice, touch, and even shared experiences.
Co-regulation helps to regulate the autonomic nervous system’s responses, promoting a shift toward the parasympathetic branch, which is associated with rest, digest, and social engagement. This can lead to increased feelings of calmness, relaxation, and emotional well-being. The social engagement system supports the ability to connect with others, form healthy relationships, and effectively navigate social interactions.
In many developmental and therapeutic contexts, co-regulation is particularly relevant. For example, in parent-child relationships, co-regulation helps infants and children develop emotional regulation skills and a secure attachment to their caregivers. Similarly, in therapeutic settings, co-regulation between a therapist and a client can create a safe and supportive environment for healing and growth.
Overall, co-regulation is a fundamental aspect of the social engagement system, enabling individuals to connect, understand, and support each other’s emotional and physiological well-being. It plays a crucial role in maintaining healthy relationships, promoting resilience, and contributing to overall social and emotional health.
Unfortunately, we live in a time when the opportunities for co-regulation are more and more difficult. This became especially important during the COVID crisis when social distancing inhibited social connectedness and mask wearing did not allow facial expressions to facilitate co-regulation.
Social Connectedness as a Biological Imperative
Dr. Porges has pointed out that social connectedness has emerged as a biological imperative, highlighting the fundamental importance of social interactions and relationships for human well-being and overall health (24).
Research across various disciplines, including psychology, neuroscience, and evolutionary biology, has emphasized the profound impact of social connectedness on human biology and physiology. From an evolutionary perspective, humans are inherently social beings, and throughout our history, social connections have played a critical role in survival and reproduction (25).
Our brains have evolved to prioritize social interactions, as they are intricately linked to our physiological and emotional well-being. The need for social connection is deeply rooted in our biology and has become an essential aspect of our overall functioning. Studies have shown that social connectedness influences a wide range of biological processes. For instance, strong social bonds and positive relationships have been associated with enhanced immune function, reduced risk of chronic diseases, and even increased longevity (26).
On the other hand, social isolation and loneliness have been linked to negative health outcomes, including increased inflammation, cardiovascular problems, and mental health issues. Social isolation and loneliness have been linked to negative health outcomes, including increased inflammation, cardiovascular problems, and mental health issues (27, 28). The biological mechanisms underlying the impact of social connectedness are multifaceted. Social interactions and meaningful relationships release hormones and neurotransmitters, such as oxytocin and serotonin, that promote feelings of trust, bonding, and happiness (29).
These neurochemicals also have regulatory effects on stress responses, immune function, and inflammation, further illustrating the intricate link between social connection and overall well-being. For example, oxytocin was found to promote health and influence behavior throughout the immune system, and it has a major role as an anti-inflammatory and antioxidant (30,31,32,33).
Furthermore, social connectedness influences our neural networks and brain structure. Research has shown that areas of the brain associated with social cognition and empathy, such as the prefrontal cortex and mirror neuron system, are activated during social interactions. These neural processes not only facilitate social understanding and empathy but also contribute to emotional regulation and resilience (34).
In today’s fast-paced and digitally connected world, it is crucial to recognize and prioritize social connectedness as a biological imperative. Building and maintaining meaningful relationships, fostering a sense of community, and engaging in positive social interactions are essential for our physical and mental health. Recognizing social connectedness as a fundamental aspect of our biology can guide us in creating supportive environments that nurture social bonds and promote well-being for individuals and societies as a whole. However, we seem to be fostering a divide between individuals by using digital interactions rather than a face-to-face connection.
Conclusion
Dr. Stephen Porges’ polyvagal theory represents a significant advancement in our understanding of the autonomic nervous system. By challenging traditional dichotomous views of the ANS, polyvagal theory provides a more comprehensive framework that integrates physiology, psychology, and social behavior. Its implications for primary care medicine hold great promise in improving patient care and fostering a deeper understanding of the complex mind-body interactions that shape our well-being.
In the next blog we will begin to explore in greater detail the implications of polyvagal theory in medicine and patient care. We will explore how polyvagal theory can enhance our understanding of patients’ physiological and behavioral responses, shedding light on various medical conditions and their connections to autonomic dysregulation. We will then evaluate the potential applications of polyvagal theory in primary care medicine, such as understanding stress-related disorders, chronic pain, gastrointestinal issues, and psychosomatic symptoms. We can then begin to highlight the importance of creating a safe and supportive therapeutic environment to promote patient well-being and enhance treatment outcomes based on polyvagal principles.
References
- Porges SW. Vagal tone: a physiologic marker of stress vulnerability. 1992; 90:498–504.
- Hering HE. A functional test of heart vagi in man. Menschen Munchen Medizinische Wochenschrift. 1910; 57:1931–1933.
- Porges SW. Respiratory sinus arrhythmia: physiological basis, quantitative methods, and clinical implications. In: Grossman P, Janssen K, Vaitl D, editors. Cardiorespiratory and Cardiosomatic Psychophysiology.Plenum; New York, NY: 1986. pp. 101–115.
- Porges SW. The polyvagal perspective. Biol Psychol. 2007; 74:116–143.
- Reed SF, Ohel G, David R, Porges SW. A neural explanation of fetal heart rate patterns: a test of the polyvagal theory. Dev Psychobiol. 1999; 35:108–118.
- Jordan D, Khalid ME, Schneiderman N, Spyer KM. The location and properties of preganglionic vagal cardiomotor neurones in the rabbit. Pflugers Arch. 1982; 395:244–250.
- Katona PG, Jih F. Respiratory sinus arrhythmia: noninvasive measure of parasympathetic cardiac control. J Appl Physiol.1975; 39:801–805.
- Porges SW. Orienting in a defensive world: mammalian modifications of our evolutionary heritage—a polyvagal theory. Psychophysiology.1995; 32:301–318.
- Porges SW. Emotion: An evolutionary by-product of the neural regulation of the autonomic nervous system. Ann N Y Acad Sci. 1997; 807:62–77.
- Porges SW. Love: An emergent property of the mammalian autonomic nervous system. Psychoneuroendocrinology. 1998; 23:837–861.
- Porges SW. The polyvagal theory: phylogenetic substrates of a social nervous system. Int J Psychophysiol. 2001; 42:123–146.
- Porges SW. Social engagement and attachment: a phylogenetic perspective. Ann N Y Acad Sci. 2003; 1008:31–47.
- Bueno L, Gue M, Fargeas MJ, Alvinerie M, Junien JL, Fioramonti J. Vagally mediated inhibition of acoustic stress-induced cortisol release by orally administered kappa-opioid substances in dogs. 1989; 124:1788–1793.
- Porges SW. The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system. Cleve Clin J Med. 2009 Apr; 76 (Suppl 2): S86-S90).
- Jackson JH. Croonian lectures on evolution and dissolution of the nervous system. Br Med J 1958; 1:591.
- Morris JL, Nilsson S. The circulatory system. In: Nilsson S, Holmgren S, editors. Comparative Physiology and Evolution of the Autonomic Nervous System.Harwood Academic Publishers; Chur, Switzerland: 1994.
- Taylor EW, Jordan D, Coote JH. Central control of the cardiovascular and respiratory systems and their interactions in vertebrates. Physiol Rev. 1999; 79:855–916.
- Morris JS, Ohman A, Dolan RJ. A subcortical pathway to the right amygdala mediating “unseen” fear. Proc Natl Acad Sci U S A.1999; 96:1680–1685.
- Porges SW. Neuroception: a subconscious system for detecting threats and safety. Zero to Three: Bulletin of the National Center for Clinical Infant Programs. 2004;24(5):19–24.
- Critchley HD. Neural mechanisms of autonomic, affective, and cognitive integration. J Comp Neurol.2005; 493:154–166.
- Porges, SW. The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation. 2011W W Norton & Co).
- Cohen, S, Janicki-Deverts, D. Can we improve our physical health by altering our social networks? Perspectives on Psychological Science, 2009; 4(4), 375-378.
- Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Annals of behavioral medicine, 2010; 40(2), 218-227.
- Porges, SW. Polyvagal Theory: A Science of Safety, Integr. Neurosci., 2022; 16:1-15.
- Alberts SC. Social influences on survival and reproduction: Insights from a long-term study of wild baboons, Journal of Animal Ecology, 2018; 88(1) 47-66.
- Yang C, Boen C, Gerken K, and Harris Social relationships and physiological determinants of longevity across the human life span, Proceedings National Academy of Sciences, 2016; 113 (3) 578-583.
- Cacioppo JT and Cacioppo S. Older adults reporting social isolation or loneliness show poorer cognitive function 4 years later, Evidence-Based Nursing 2014;17(2):59-60.
- Eating, H.Social isolation, loneliness in older people pose health risks, National Institute on Aging, News and Events. 4/23/2019.